BY RAINBOW ZHAO
1. Introduction
The human body comprises various organs, including the stomach, liver, and lungs (Wakim and Grewal, 2018). However, none of these organs can function without energy, specifically adenosine triphosphate (ATP) produced during cell respiration (BBC Bitesize, 2018). Of the two types of cell respiration, aerobic respiration allows for the mass production of ATP (BBC Bitesize, 2024). During this process, O2 acts as an essential electron acceptor (Babcock, 1999). In essence, O2 serves an unwavering purpose for every organ. But which organ ensures that oxygen is delivered to all the others? The heart.
2. Anatomy and the Cardiac Cycle
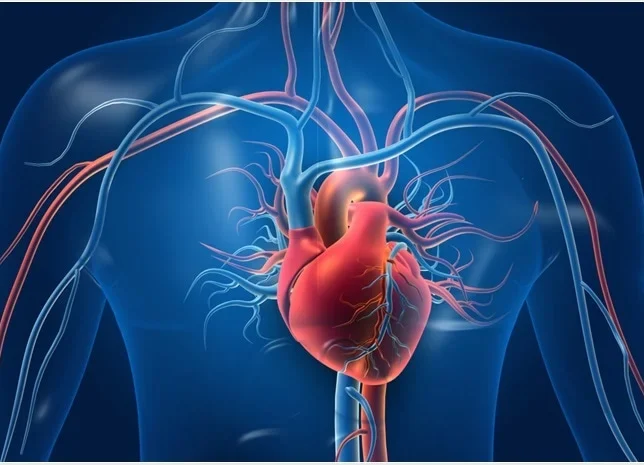
The heart is located behind the sternum and in between the lungs (Cleveland Clinic, 2024; Texas Heart Institute, 2024). It is the main organ of the cardiovascular system, with the role of pumping blood throughout the body (Chaudhry et al., 2023). The heart consists of four chambers: left and right atria and ventricles (ibid). The right atrium and ventricle receives deoxygenated blood and pumps it through the pulmonary arteries to the lungs for oxygenation of the blood (Pollock and Makaryus, 2021). Afterwards, oxygenated blood comes back through the pulmonary veins into the left atrium, and the left ventricle pumps the oxygenated blood into the aorta, delivering oxygen to the rest of the body (ibid).
Figure 1: A labeled diagram of the heart demonstrating the cardiac cycle (adapted from: Learn How the Heart Beats 2010).
3. Cardiomyocytes
Cardiomyocytes constitute approximately 30% of the heart’s cells, while accounting for about 70-85% of the heart’s volume (Dewing et al., 2022). There are two main types of cardiomyocytes: pacemaker and contractile (Gopalan and Kirk, 2022). In reality, the heart pumps blood by contracting, and this is achieved through contractile cardiomyocytes. On the other hand, pacemaker cardiomyocytes, or cells, don’t contract (Jakoi, 2024). Instead, they serve a different purpose.
The heart is often described as myogenic, meaning the signal of contraction, or action potential, originates in the heart itself (Encyclopedia Britannica, 2024). The pacemaker cells are the ones capable of intrinsically generating action potentials. There are five main locations of pacemaker cells: sinoatrial (SA) node, atrioventricular (AV) node, bundle of His, bundle branches, and Purkinje fibres (Metkus, 2022).
Figure 2: A labeled diagram of the heart showing the main locations of pacemaker cells (adapted from: EKG, ECG Interpretation, 2024)
4. The Intrinsic Conduction System and the Heart’s Myogenic Nature
4.1 Initiating the Action Potential
The intrinsic conduction system establishes the base sinus rhythm of the heart (Bhattacharyya and Munshi, 2020). The SA node is located in the right atria (Kashou et al., 2022). It serves as the primary pacemaker-region of the heart, containing lots of pacemaker cells (ibid). These cells are abundant in hyperpolarization-activated cyclic nucleotide–gated (HCN) channels, specifically HCN4 channels (Hennis et al., 2022). These channels are voltage-gated, and they open upon hyperpolarization (Sartiani et al., 2017). This implies that they are ‘leaky’ during the resting membrane potential of -60 mV (Levick, 1991). Once the HCN channels open, Na+ can enter the cell, bringing the membrane potential from -60 mV to approximately -55 mV (Manoj et al., 2023). This causes the opening of another voltage-gated channel called T-type calcium channels (TTCC) (ibid). They allow the inflow of a limited amount of Ca2+to bring the membrane potential to -40 mV, enough to trigger the action potential (Ono and Iijima, 2005). At this point, a third type of voltage-gated channel called L-type calcium channel (LTCC) opens up, bringing the membrane potential to +40 mV with a significant influx of Ca2+(Satin and Schrode, 2009).
4.2 Propagation of the Action Potential
The cell is now abundant in Ca2+. In reality, specialized junctions called intercalated discs link cardiomyocytes together (Bennett, 2018). One very important component of the intercalated disc is the gap junction (Sun et al., 2020). The gap junction is made up of channels called connexons (Mammano, 2013). With the presence of connexons, Ca2+in the pacemaker cell can diffuse into other nearby pacemaker cells, allowing the action potential to propagate to the other four pacemaker regions (ibid). Along the way, Ca2+ can also diffuse into nearby contractile cardiomyocytes to trigger contraction (ibid). The specific mechanism of this isn’t too dissimilar from that of skeletal muscles, however, it is not the main focus of this article.
Figure 3: A labeled diagram of cardiomyocytes showing gap junctions within intercalated discs (adapted from: Cardiac Muscle Tissue, 2024).
4.3 Alternative Pacemakers
The SA node establishes a base sinus rhythm of 60-100 bpm (Kashou et al., 2022). When the SA node fails due to various reasons such as diseases, the AV node takes over as the secondary pacemaker (Hafeez and Grossman, 2020). The AV node, bundle of His, and bundle branches can establish a base rhythm of 40-60 bpm, whereas Purkinje fibres can establish a base rhythm of 20-40 bpm (sites.pitt.edu, 2024). Although not ideal, these pacemaker cells can serve as a temporary backup if the SA node were to fail, ensuring that blood circulation can still occur.
5. The Extrinsic Conduction System and the Regulation of Heart Rate
5.1 The Autonomic Nervous System (ANS)
Although the heart is described as myogenic, regulation of the heart rate still relies on the extrinsic conduction system. There are two main regulators of heart rate, including the autonomic nervous system (ANS) and hormones such as epinephrine (Mano et al., 1991). The role of the ANS in regulating heart rate will be explained in greater detail. However, the hormonal regulation mechanism only differs primarily in that hormones act as ligands rather than neurotransmitters.
The ANS is part of the peripheral nervous system in charge of regulating involuntary physiological processes (Waxenbaum et al., 2023). It is composed of three divisions, including the sympathetic nervous system (SNS), parasympathetic nervous system (PNS), and enteric nervous system (ENS) (ibid). SNS and PNS are the ones regulating heart rate (ibid). The SNS is mainly in charge of elevated activity, or ‘fight or flight’ response, whereas the PNS is in charge of relaxation, or ‘rest or digest’ processes (ibid). Therefore, it is evident that SNS helps increase the heart rate, while PNS helps decrease the heart rate.
5.2 Sympathetic Nervous System (SNS) Increasing Heart Rate
The SNS releases norepinephrine, which stimulates a type of G protein-coupled receptor (GPCR) called the beta-1 adrenergic receptors (β1-AR) located on the plasma membrane of pacemaker cells along with epinephrine released from the adrenal medulla (Bylund, 2009; Cleveland Clinic, 2022; Vasudevan et al., 2011). β1-AR then activates a stimulatory G protein (Gs) (Pandey et al., 2020). Gs has three subunits, including α, β, and γ (Purves et al., 2001). Normally, the α subunit is bound to GDP (ibid). However, when activated, the Gαs releases its guanosine diphosphate (GDP) and instead binds to guanosine triphosphate (GTP) (ibid). This results in the dissociation of the Gαs-GTP complex from the βγ dimer (ibid).
The Gαs-GTP complex is now free to interact with and stimulate an effector enzyme called adenylyl cyclase (AC) located on the plasma membrane of the pacemaker cell (Purves et al., 2001). AC is capable of hydrolyzing ATP into cyclic adenosine monophosphate (cAMP), which in turn is capable of activating protein kinase A (PKA) (Kuszak and Sunahara, 2010). Finally, PKA phosphorylates, in other words, stimulate LTCC, resulting in the increased influx of Ca2+ into the pacemaker cell (Liu et al., 2021). This makes it easier for the cell to depolarize again even after hyperpolarization, and hence, result in more frequent action potentials. As a result, the rate of contraction of the cardiomyocyte increases, and ultimately, the heart rate increases.
5.3 Parasympathetic Nervous System (PNS) Decreasing Heart Rate
On the contrary, the PNS releases acetylcholine (Tindle and Tadi, 2022). Acetylcholine stimulates another type of GPCR called the M2 muscarinic receptors (M2-R) located on the plasma membrane of pacemaker cells (ibid). This time, M2-R activates an inhibitory G protein (Gi) with 3 subunits, including αi, β, and γ (Harvey and Calaghan, 2012; Villaseca et al., 2022). Identical to what happens with the stimulatory pathway, Gαi releases GDP in exchange for GTP, leading to the dissociation of the Gαi-GTP complex from the βγ dimer (Harvey and Calaghan, 2012).
However, in the inhibitory pathway, the Gαi-GTP complex can interact with and inhibit AC (Harvey and Calaghan, 2012). This results in the decrease of intracellular Ca2+levels. Moreover, the βγ dimer also dissociates from the Gi (Ang et al., 2012). They can directly interact and open G protein-gated inwardly rectifying potassium (GIRK) channels located on the plasma membrane of pacemaker cells (ibid). When these channels open, K+ can exit the cells, causing the cell to hyperpolarize. When the cell hyperpolarizes, it becomes harder to depolarize again. Thus, action potentials will be generated less frequently, resulting in the decrease of the rate of cardiomyocyte contraction, decreasing the heart rate.
Figure 4: A visual representation of the mechanism regulating the heart rate (adapted from: Cardiac Signal Transduction Mechanisms (G-Protein-Linked), 2024)
It is also worth noting that although the βγ dimer also dissociates from Gs in the stimulatory pathway, it doesn’t typically interact with GIRK as that would be counter-intuitive (Tennakoon et al., 2021). Instead, it is involved in other important steps of the signaling process, such as membrane anchoring, ensuring all the essential components are at the correct location during the process (Koch et al., 1993).
6. Importance of the Heart’s Regulatory Functions
The regulatory functions of the heart serve a variety of purposes. The most obvious one is supplying the rest of the body with an appropriate amount of O2 and nutrients under any given circumstances to maintain homeostasis, whether that is during sleep or exercise (Information, 2019). During exercise, the body, especially the skeletal muscles, is in demand of more nutrients such as glucose and O2(Hargreaves et al., 2020). In order to meet this demand, the rate of gas exchange needs to increase, as well as the rate of blood flow (James, 2022). Therefore, the heart rate must also increase to meet this demand (ibid). Conversely, during sleep, the body demands less energy, therefore, there is no need to generate and expand excess energy (Cleveland Clinic, 2023). Hence, the heart rate decreases.
Additionally, this also implies that waste products like CO2from cell respiration are removed consistently (Patel et al., 2022). CO2 dissolves in H2O (which makes up nearly 90% of the blood plasma and 50% of the blood) to form HCO3– and H+, especially with the help of carbonic anhydrase in erythrocytes (Boron, 2020; National Cancer Institute, 2020). If CO2is not excreted from the body consistently at a sufficient level, blood pH can drop to a considerable extent with the presence of H+(Patel et al., 2022). This can lead to hypercarbia, with symptoms such as headache, depression, and confusion (Cleveland Clinic, 2023).
Another very important reason to regulate heart rate is to control the blood pressure (Reule and Drawz, 2012). When the heart rate is too high, this can generally lead to elevated blood pressure (ibid). The opposite leads to low blood pressure (American Heart Association, 2023). If the heart rate isn’t regulated properly, conditions such as hypertension and hypotension may result (British Heart Foundation, 2024; Reule and Drawz, 2012).
7. Conclusion
The heart plays a crucial role in the body, controlling blood flow and thereby ensuring the proper delivery of nutrients and O2to all other organs, as well as maintaining homeostasis. This is accomplished by pacemaker cells setting a base sinus rhythm, with the ANS regulating it by releasing neurotransmitters such as acetylcholine and norepinephrine, thereby triggering a cascade of regulatory mechanisms. After a deep dive into the detailed mechanism behind the heart’s incredible myogenic nature, it is evident that any disruptions in these complex mechanisms can lead to a variety of health conditions, whether that has to do with the heart itself or all the other parts of the body that the heart serves. Therefore, understanding these processes offers a powerful reminder to prioritize heart health, as it is essential to our overall well-being.
8. Bibliography
American Heart Association (2023). Low Blood Pressure – When Blood Pressure Is Too Low. [online] www.heart.org. Available at:
https://www.heart.org/en/health-topics/high-blood-pressure/the-facts-about-high-blood-pressure/ low-blood-pressure-when-blood-pressure-is-too-low.
Ang, R., Opel, A. and Tinker, A. (2012). The Role of Inhibitory G Proteins and Regulators of G Protein Signaling in the in vivo Control of Heart Rate and Predisposition to Cardiac Arrhythmias. Frontiers in Physiology, [online] 3. doi:https://doi.org/10.3389/fphys.2012.00096.
Babcock, G.T. (1999). How oxygen is activated and reduced in respiration. Proceedings of the National Academy of Sciences of the United States of America, [online] 96(23), pp.12971–12973. Available at: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC33932/.
Bailey, R. (2010). Learn How the Heart Beats. [online] ThoughtCo. Available at: https://www.thoughtco.com/phases-of-the-cardiac-cycle-anatomy-373240.
BBC Bitesize (2018). Cellular respiration – Respiration – OCR Gateway – GCSE Biology (Single Science) Revision – OCR Gateway – BBC Bitesize. [online] BBC Bitesize. Available at: https://www.bbc.co.uk/bitesize/guides/zwghcj6/revision/1#:~:text=Every%20cell%20in%20a%20l iving [Accessed 9 Aug. 2024].
BBC Bitesize. (n.d.). What is the difference between aerobic and anaerobic respiration? [online] Available at:
https://www.bbc.co.uk/bitesize/articles/zdqx2v4#:~:text=Respiration%20is%20a%20chemical%2 0reaction.
Bennett, P.M. (2018). Riding the waves of the intercalated disc of the heart. Biophysical Reviews, 10(4), pp.955–959. doi:https://doi.org/10.1007/s12551-018-0438-z.
Bhattacharyya, S. and Munshi, N.V. (2020). Development of the Cardiac Conduction System. Cold Spring Harbor Perspectives in Biology, 12(12), p.a037408.
doi:https://doi.org/10.1101/cshperspect.a037408.
Boron, W.F. (2010). Evaluating the role of carbonic anhydrases in the transport of HCO3−-related species. Biochimica et biophysica acta, [online] 1804(2), pp.410–421. doi:https://doi.org/10.1016/j.bbapap.2009.10.021.
Cleveland Clinic (2023). Hypercapnia. [online] Cleveland Clinic. Available at: https://my.clevelandclinic.org/health/diseases/24808-hypercapnia.
British Heart Foundation (2024). Low blood pressure. [online] Bhf.org.uk. Available at: https://www.bhf.org.uk/informationsupport/heart-matters-magazine/medical/low-blood-pressure# :~:text=If%20your%20heart%20rate%20does.
Bylund, D.B. (2009). Norepinephrine: Adrenergic Receptors. Encyclopedia of Neuroscience, pp.1231–1236. doi:https://doi.org/10.1016/b978-008045046-9.01154-2.
ceufast.com. (n.d.). EKG, ECG Interpretation. [online] Available at:
https://ceufast.com/course/ecg-interpretation.
Chaudhry, R., Miao, J.H. and Rehman, A. (2023). Physiology, Cardiovascular. [online] PubMed. Available at:
https://www.ncbi.nlm.nih.gov/books/NBK493197/#:~:text=The%20heart%20is%20the%20organ.
Cleveland Clinic (2022). Adrenal Medulla: What It Is, Function & Diseases. [online] Cleveland Clinic. Available at: https://my.clevelandclinic.org/health/body/23034-adrenal-medulla.
Cleveland Clinic (2024). Heart: Anatomy and Function. [online] Cleveland Clinic. Available at: https://my.clevelandclinic.org/health/body/21704-heart.
Cleveland Clinic. (2023). Sleep. [online] Available at:
https://my.clevelandclinic.org/health/body/12148-sleep-basics.
cvphysiology.com. (n.d.). CV Physiology | Cardiac Signal Transduction Mechanisms (G-Protein-Linked). [online] Available at: https://cvphysiology.com/blood-pressure/bp011a.
Wakim, S. and Grewal, M. (2018). 10.4: Human Organs and Organ Systems. [online] Biology LibreTexts. Available at:
https://bio.libretexts.org/Bookshelves/Human_Biology/Human_Biology_(Wakim_and_Grewal)/10 %3A_Introduction_to_the_Human_Body/10.4%3A_Human_Organs_and_Organ_Systems.
Dewing, J.M., Saunders, V., Ita O’Kelly and Wilson, D.I. (2022). Defining cardiac cell populations and relative cellular composition of the early fetal human heart. 17(11), pp.e0259477–e0259477. doi:https://doi.org/10.1371/journal.pone.0259477.
Encyclopedia Britannica. (n.d.). Circulatory system – Body fluids. [online] Available at: https://www.britannica.com/science/circulatory-system/Body-fluids#ref106157.
Gopalan, C. and Kirk, E. (2022). Chapter 1 – The heart. [online] ScienceDirect. Available at: https://www.sciencedirect.com/science/article/abs/pii/B9780128234211000111.
Hafeez, Y. and Grossman, S.A. (2020). Junctional Rhythm. [online] PubMed. Available at: https://www.ncbi.nlm.nih.gov/books/NBK507715/.
Hargreaves, M. and Spriet, L.L. (2020). Skeletal muscle energy metabolism during exercise. Nature Metabolism, 2(9), pp.817–828. doi:https://doi.org/10.1038/s42255-020-0251-4.
Harvey, R.D. and Calaghan, S.C. (2012). Caveolae create local signalling domains through their distinct protein content, lipid profile and morphology. Journal of Molecular and Cellular Cardiology, [online] 52(2), pp.366–375. doi:https://doi.org/10.1016/j.yjmcc.2011.07.007.
Hennis, K., Biel, M., Fenske, S. and Wahl-Schott, C. (2022). Paradigm shift: new concepts for HCN4 function in cardiac pacemaking. Pflügers Archiv – European Journal of Physiology. doi:https://doi.org/10.1007/s00424-022-02698-4.
Information, N.C. for B., Pike, U.S.N.L. of M. 8600 R., MD, B. and Usa, 20894 (2019). How does the heart work? [online] www.ncbi.nlm.nih.gov. Institute for Quality and Efficiency in Health Care (IQWiG). Available at: https://www.ncbi.nlm.nih.gov/books/NBK279249/.
Jakoi, E. (n.d.). CV 1. HEART ELECTRICAL ACTIVTY LEARNING OBJECTIVES. [online] Introductory Human Physiology. Available at:
https://histology.oit.duke.edu/MBS/Videos/Phys/Phys%204.1%20CV%20Heart%20Electrical/Ph ys%204.1%20CV%20Heart%20Electrical%20NOTES.pdf.
James, A. (2022). Responses of The Respiratory System to Stress – Exercise – Altitude. [online] TeachMePhysiology. Available at:
https://teachmephysiology.com/respiratory-system/regulation/responses-respiratory-system-stre ss/#:~:text=During%20exercise%2C%20the%20gas%20exchange.
Kashou, A.H., Basit, H. and Chhabra, L. (2022). Physiology, Sinoatrial Node. [online] PubMed. Available at:
https://www.ncbi.nlm.nih.gov/books/NBK459238/#:~:text=The%20SA%20node%2C%20also%2 0known.
Koch, W.J., Inglese, J., Stone, W.C. and Lefkowitz, R.J. (1993). The binding site for the beta gamma subunits of heterotrimeric G proteins on the beta-adrenergic receptor kinase. Journal of Biological Chemistry, 268(11), pp.8256–8260.
doi:https://doi.org/10.1016/s0021-9258(18)53090-8.
Kuszak, A.J. and Sunahara, R.K. (2010). Adenylyl Cyclases. Elsevier eBooks, pp.1389–1397. doi:https://doi.org/10.1016/b978-0-12-374145-5.00171-6.
Levick, J.R. (1991). Cardiac excitation and contraction. An Introduction to Cardiovascular Physiology, pp.23–44. doi:https://doi.org/10.1016/b978-0-7506-1028-5.50006-8.
Liu, Y., Chen, J., Fontes, S.K., Bautista, E.N. and Cheng, Z. (2021). Physiological and pathological roles of protein kinase A in the heart. Cardiovascular Research, 118(2). doi:https://doi.org/10.1093/cvr/cvab008.
Mammano, F. (2013). Gap Junctions: Cell-Cell Channels in Animals. [online] www.ncbi.nlm.nih.gov. Available at: https://www.ncbi.nlm.nih.gov/books/NBK6455/.
Mano, T., Iwase, S., Saito, M., Koga, K., Abe, H., Inamura, K. and Matsukawa, T. (1991). Neural and humoral controlling mechanisms of cardiovascular functions in man under weightlessness simulated by water immersion. Acta Astronautica, [online] 23, pp.31–33.
doi:https://doi.org/10.1016/0094-5765(91)90096-n.
Manoj, P., Kim, J.A., Kim, S., Li, T., Sewani, M., Chelu, M.G. and Li, N. (2023). Sinus node dysfunction: current understanding and future directions. American Journal of Physiology-Heart and Circulatory Physiology, 324(3), pp.H259–H278.
doi:https://doi.org/10.1152/ajpheart.00618.2022.
Metkus, T. (2022). Cardiac conduction system – Health Video: MedlinePlus Medical Encyclopedia. [online] Medlineplus.gov. Available at:
https://medlineplus.gov/ency/anatomyvideos/000021.htm.
National Cancer Institute (2020). Composition of the Blood | SEER Training. [online] Cancer.gov. Available at: https://training.seer.cancer.gov/leukemia/anatomy/composition.html.
Ono, K. and Iijima, T. (2005). Pathophysiological Significance of T-type Ca2+ Channels: Properties and Functional Roles of T-type Ca2+ Channels in Cardiac Pacemaking. Journal of Pharmacological Sciences, 99(3), pp.197–204. doi:https://doi.org/10.1254/jphs.fmj05002x2.
Pandey, S., Saha, S. and Shukla, A.K. (2020). Transmitting the Signal: Structure of the β1-Adrenergic Receptor-Gs Protein Complex. Molecular Cell, 80(1), pp.3–5. doi:https://doi.org/10.1016/j.molcel.2020.09.016.
Patel, S., Miao, J.H., Yetiskul, E., Anokhin, A. and Majmundar, S.H. (2022). Physiology, Carbon Dioxide Retention. [online] PubMed. Available at:
https://www.ncbi.nlm.nih.gov/books/NBK482456/#:~:text=CO2%20is%20transported%20in%20t he.
Pinterest. (2024). Cardiac Muscle Tissue [online] Available at:
https://www.pinterest.com/pin/796785359067603048/ [Accessed 9 Aug. 2024].
Pollock, J.D. and Makaryus, A.N. (2021). Physiology, Cardiac Cycle. [online] PubMed. Available at:
https://www.ncbi.nlm.nih.gov/books/NBK459327/#:~:text=The%20cardiac%20cycle%20is%20a. 11
Purves, D., Augustine, G.J., Fitzpatrick, D., Katz, L.C., LaMantia, A.-S., McNamara, J.O. and Williams, S.M. (2001). G-Proteins and Their Molecular Targets. [online] www.ncbi.nlm.nih.gov. Available at:
https://www.ncbi.nlm.nih.gov/books/NBK10832/#:~:text=Heterotrimeric%20G%2Dproteins%20ar e%20composed.
Reule, S. and Drawz, P.E. (2012). Heart Rate and Blood Pressure: Any Possible Implications for Management of Hypertension? Current Hypertension Reports, 14(6), pp.478–484. doi:https://doi.org/10.1007/s11906-012-0306-3.
Sartiani, L., Mannaioni, G., Masi, A., Novella Romanelli, M. and Cerbai, E. (2017). The Hyperpolarization-Activated Cyclic Nucleotide-Gated Channels: from Biophysics to Pharmacology of a Unique Family of Ion Channels. Pharmacological Reviews, [online] 69(4), pp.354–395. doi:https://doi.org/10.1124/pr.117.014035.
Satin, J. and Schroder, E.A. (2009). Autoregulation of Cardiac l-Type Calcium Channels. Trends in Cardiovascular Medicine, [online] 19(8), pp.268–271.
doi:https://doi.org/10.1016/j.tcm.2010.02.009.
sites.pitt.edu. (n.d.). Cardiac Arrythmia Webquest > Process > Cardiac Conduction System > start. [online] Available at:
https://sites.pitt.edu/~jet10/process/conduction_system/conduction_index.htm.
Sun, Y., Lee, S.-M., Ku, B.-J. and Moon, M.-J. (2020). Fine structure of the intercalated disc and cardiac junctions in the black widow spider Latrodectus mactans. Applied Microscopy, [online] 50(1). doi:https://doi.org/10.1186/s42649-020-00040-9.
Tennakoon, M., Senarath, K., Kankanamge, D., Ratnayake, K., Wijayaratna, D., Olupothage, K., Ubeysinghe, S., Martins-Cannavino, K., Hébert, T.E. and Karunarathne, A. (2021). Subtype-dependent regulation of Gβγ signalling. Cellular Signalling, 82, p.109947. doi:https://doi.org/10.1016/j.cellsig.2021.109947.
Texas Heart Institute. (n.d.). Heart Information Center: Heart Anatomy. [online] Available at: https://www.texasheart.org/heart-health/heart-information-center/topics/heart-anatomy/#:~:text=l iters)%20of%20blood.-.
Tindle, J. and Tadi, P. (2022). Neuroanatomy, Parasympathetic Nervous System. [online] PubMed. Available at: https://www.ncbi.nlm.nih.gov/books/NBK553141/.
Vasudevan, N.T., Mohan, M.L., Goswami, S.K. and Naga Prasad, S.V. (2011). Regulation of β-adrenergic receptor function. Cell Cycle, [online] 10(21), pp.3684–3691. doi:https://doi.org/10.4161/cc.10.21.18042.
Villaseca, S., Romero, G., Ruiz, M.-J., Carlos Pérez García‐Pando, Leal, J.I., Tovar, L.M. and Torrejón, M. (2022). Gαi protein subunit: A step toward understanding its non-canonical mechanisms. Frontiers in Cell and Developmental Biology, 10.
doi:https://doi.org/10.3389/fcell.2022.941870.
Waxenbaum, J.A., Reddy, V. and Varacallo, M. (2023). Anatomy, Autonomic Nervous System. [online] PubMed. Available at:
https://www.ncbi.nlm.nih.gov/books/NBK539845/#:~:text=The%20autonomic%20nervous%20sy stem%20is.