BY IBRAHEEM MANDA
Parkinson’s Disease: An Introduction
Parkinson’s is a neurodegenerative disease that affects the elderly population the most. Its symptoms can be classed into physical and cognitive. In this article, I will be focusing on how Parkinson’s affects brain function and what medications do to treat it from a neurological perspective followed by the future of treatment for Parkinson’s and other neurodegenerative diseases.
The Progression of Parksinson’s
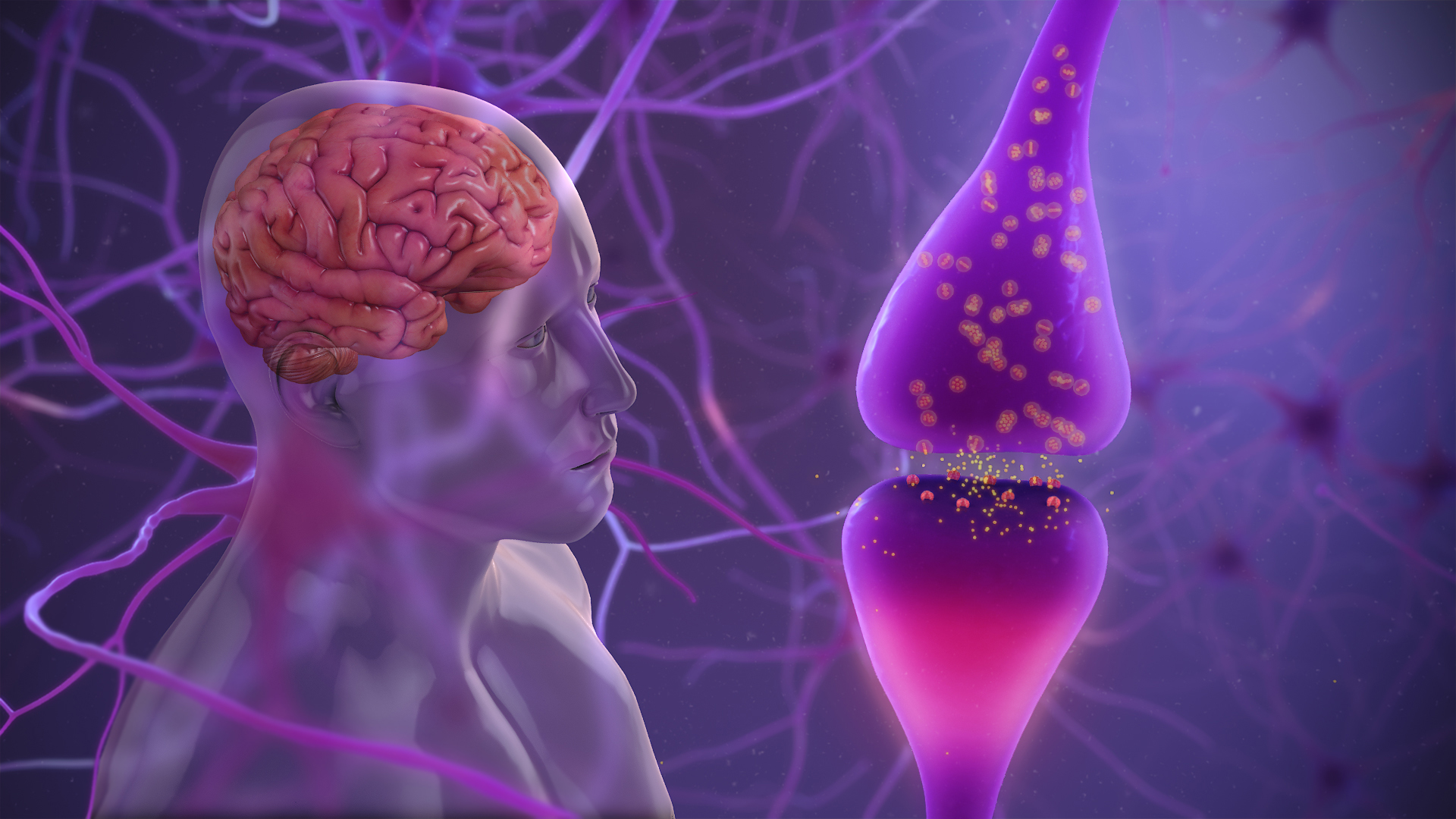
Parkinson’s disease originates from a region in the brain called the Substantia Nigra. Dopaminergic neurones start to deteriorate, this could be due to Lewy bodies (misfolded proteins), mitochondrial misfunction and neuroinflammation. This causes dopamine levels to fall, which reduces the amount of communication between the neocortex and the striatum, this means reduced motor neurone activity, and hence this is where mobility symptoms come in. When these dopamine levels fall, GABA levels increase (which acts a sedative and inhibits some neurological activity) and this leads ACH levels to increase. This stimulates cholinergic and motor neurones, which leads to symptoms such as lack of smooth movement, tremors, and difficulty in co-ordination. As time progresses, movement becomes increasingly difficult and can eventually lead to heavily impaired motor function, and rarely paralysis.
Inside the Medicine Cabinet: How Parkinson’s Drugs Work
To treat the symptoms of Parkinson’s, dopamine levels must be replenished. Dopamine cannot be given directly due to the blood brain barrier which prevents dopamine from entering the brain by an extremely selectively permeable membrane made of epithelial cells, Hence L-dopa or levodopa must be given, as this will not be blocked by the blood-brain barrier. Levodopa is given alongside carbidopa and entacapone. This prevents Levodopa being broken down into 3-OMD and dopamine before it reaches the correct region of the brain.
Levodopa is then broken down by AADC into dopamine once it enters the substantia nigra. This replenishment of dopamine prevents GABA and ACH increasing, and helps with restoring movement ability as motor neurone activity increases.
Anticholinergic agents such as benztropine and biperiden helps to reduce the effect of ACH by binding to muscarinic receptors. This reduces the effect of increased ACH such as tremors and involuntary movement.
GABAPENTIN reduces the release of exciting neurotransmitters such as glutamate. This can reduce symptoms such as nerve pain and restless leg syndrome.
Bromocriptine and Ropinirole are also sometimes given, which are dopamine agonists, that directly stimulate dopamine receptors, and hence helps with movement and hormone regulation, although can result in impulse control issues.
All of these medications focus on amending the symptoms of Parkinson’s, but none can reverse the damage that has been caused, at most they slow the development of symptoms.
With degenerative diseases the goal should be to revert damage done, but the brain 4 in a way that is unique to it as an organ. For a smoker if they quite, most of their lung damage is reverted after about 10-15 years, as cells can easily regenerate and repair, but this does not apply to the brain. Scientists are testing therapies that hope to revert damage, although none of such seem to be available soon.
Beyond Today: The Future of Parkinson’s Treatment
Future treatments of Parkinson’s focus on restoring the dopaminergic neurones or stimulating/inhibiting certain neurones without affecting other parts of the brain.
Gene and stem-cell therapies both aim to restore neurone functions in different ways. Gene therapy aims to deliver genes that can produce proteins beneficial for dopamine production or enhance neurone survival. Stem cell therapy on the other aims to regenerate damaged dopaminergic neurons in the substantia nigra through transplanting stem cell or using induced pluripotent stem cells (IPSC’s). Both of these treatments aim to prevent symptoms of Parkinson’s before they begin.
New medication such as glutamate modulators, neuroprotective agents are being researched and may be used in future treatment. Glutamate modulators alleviate dyskinesia and other motor symptoms without affecting dopamine levels, which can lead to less severe side effects, which is a key issue with having many medications to treat a disease like Parkinson’s. Researchers are identifying neuroprotective agents which help to slow disease progression by preventing the dysfunction of key dopaminergic neurones.
Gene therapy, although mostly in the experimental stage, has started trials such as the AAV2-GDNF (glial cell-derived neurotrophic factor) which is not widely available but is being investigated is several trials. If proven effective, Gene therapy offers a long-lasting solution for otherwise untreatable patients.
Conclusion
The brain has always been a very mysterious organ, and hence when time comes for treatment, some things remain a mystery. Some of these mysteries include why Lewy bodies are produced, or why neurones in the substantia nigra are likely to degenerate first. Many injuries and diseases are able to heal/repair on their own, but with the brain, it has a very limited ability to repair/reorganise after injury or disease, this is known (or not well known enough) as neuroplasticity.
Parkinson’s by nature is a disease which requires close monitoring and early detection. If you know anyone that shows any of the symptoms mentioned in this article and fits the elderly age group, reach out to your local GP, or contact 111 (UK) or your nation’s non-emergency health line.
Glossary
Dopaminergic: Referring to neurons or pathways in the brain that release or are activated by dopamine.
Lewy bodies: Abnormal aggregates of protein that develop inside nerve cells, often associated with Parkinson’s disease and dementia.
GABA (Gamma-Aminobutyric Acid): A neurotransmitter that inhibits nerve transmission in the brain, helping to regulate neuronal excitability.
ACH (Acetylcholine): A neurotransmitter involved in muscle activation and various brain functions, including attention and memory.
Cholinergic: Pertaining to nerve cells or synapses that use acetylcholine as their neurotransmitter.
L-Dopa (Levodopa): A precursor to dopamine used in the treatment of Parkinson’s disease to replenish brain dopamine levels.
Entacapone: A medication that inhibits the enzyme COMT (catechol-O-methyltransferase), prolonging the effect of L-Dopa by reducing its breakdown.
Carbidopa: A drug that prevents the conversion of L-Dopa into dopamine outside the brain, ensuring more L-Dopa reaches the brain and minimizing side effects.
3-OMD (3-O-methyldopa): A byproduct of L-Dopa metabolism that competes with L-Dopa for transport across the blood-brain barrier.
AADC (Aromatic L-amino Acid Decarboxylase): An enzyme responsible for converting L-Dopa into dopamine in the brain.
Benztropine: An anticholinergic drug used to reduce tremors and muscle stiffness in Parkinson’s disease by blocking acetylcholine activity.
Biperiden: An anticholinergic medication used to treat symptoms of Parkinson’s disease by reducing muscle rigidity and tremors.
Gabapentin: A drug that modulates the activity of certain neurotransmitters and is sometimes used off-label for managing symptoms such as tremors in Parkinson’s disease.
Bromocriptine: A dopamine agonist that stimulates dopamine receptors in the brain and is used to treat Parkinson’s disease and other conditions.
Ropinirole: A dopamine agonist that mimics the action of dopamine and is used to manage the symptoms of Parkinson’s disease.
Sources/citations
• National Health Service (2022). Symptoms – Parkinson’s disease. [Online] NHS. Available at: https://www.nhs.uk/conditions/parkinsons-disease/symptoms/.
• NHS (2022). Parkinson’s disease – Causes. Available at: https://www.nhs.uk/conditions/parkinsons-disease/causes/ (Accessed: 19 October 2024).
• NICE (2023). Co-careldopa and Co-beneldopa (Levodopa) – British National Formulary (BNF). Available at: https://bnf.nice.org.uk/drug/co-careldopa.html (Accessed: 19 October 2024).
• NHS (2023). Levodopa and carbidopa. Available at: NHS (Accessed: 19 October 2024).
• BNF (2024). Levodopa with carbidopa. Available at: BNF (Accessed: 19 October 2024).
• NHS (2022). Gabapentin: Uses, Side Effects, and How It Works. Available at: https://www.nhs.uk/medicines/gabapentin/ (Accessed: 19 October 2024).
• NHS (2023). Gabapentin. Available at: NHS (Accessed: 19 October 2024).
• BNF (2024). Gabapentin. Available at: BNF (Accessed: 19 October 2024).
• NICE (2023). Lorazepam – British National Formulary (BNF). Available at: https://bnf.nice.org.uk/drug/lorazepam.html (Accessed: 19 October 2024).
• NHS (2023). About lorazepam. Available at: NHS (Accessed: 19 October 2024).
• BNF (2024). Lorazepam. Available at: BNF (Accessed: 19 October 2024).
• NICE (2023). Controlled Drugs and Drug Dependence. Available at: NICE (Accessed: 19 October 2024).
• Nussbaum, R.L. and Ellis, C.E. (2003). Cerebral dopamine neurotrophic factor: A new gene therapy for Parkinson’s disease. Nature Reviews Neuroscience, 4(7), pp. 578-588. doi:10.1038/nrn1150.
• Lindvall, O. and Kokaia, Z. (2006). Stem cell therapy for human neurodegenerative disorders—how to make it work. Nature Reviews Neuroscience, 7(5), pp. 324-330. doi:10.1038/nrn1908.
• Fox, S.H., et al. (2018). Glutamate and Parkinson’s disease. Movement Disorders, 33(9), pp. 1360-1370. doi:10.1002/mds.27334.
• Olanow, C.W., et al. (2009). A double-blind, randomized, placebo-controlled trial of rasagiline in early Parkinson’s disease. Neurology, 72(3), pp. 214-221. doi:10.1212/01.wnl.0000330245.43657.02.
• Parkinson’s UK (n.d.). Levodopa, Co-beneldopa, and Co-careldopa. Available at: https://www.parkinsons.org.uk/information-and-support/levodopa-co-beneldopa-and-co-careldopa#:~:text=How%20do%20levodopa%20drugs%20work,cells%20can%20make%20more%20dopamine./
• Speed Pharmacology – Parkinson’s Made Easy. (n.d.). Available at: https://youtu.be/Z84iypHdftQ?si=-CrKTzxXsfQLnboG.