By: Aidan Fu ([email protected])
- Introduction
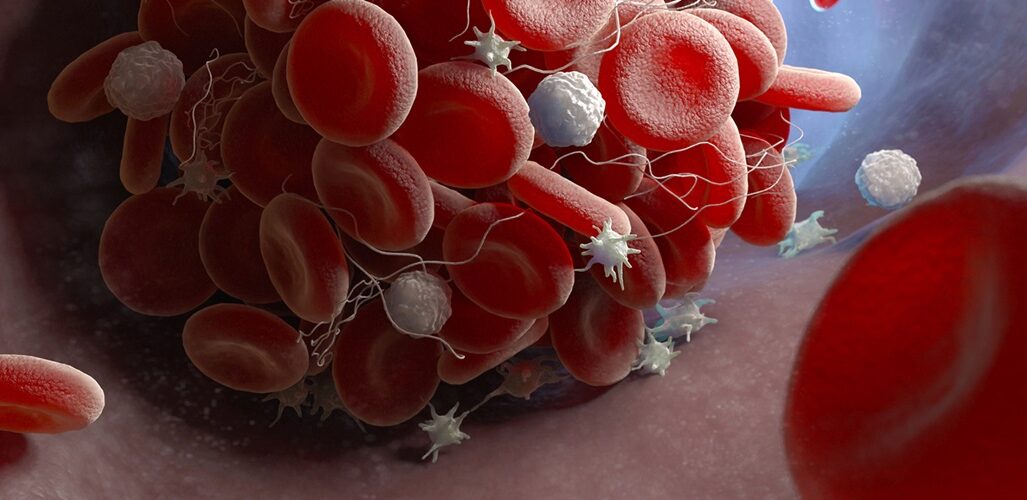
Platelets play a crucial role in forming ‘scabs’ and plugging wounds, a process vital for healing (University of Rochester Medical Center, 2019). Platelet-rich Plasma (PRP) involves extracting blood from the body and spinning it in a centrifuge to separate red and white blood cells, creating a concentrated solution rich in platelets (Platelet-Rich Plasma (PRP) Injection: How It Works | HSS, 2015).Many athletes use these injections as they stimulate the healing process and provide specific growth factors to speed up recovery time (Yale Medicine, n.d.).
- Conservative Alternative for Tears
Traditionally, athletes with strained or torn tendons require surgery to repair the damage (MSD Manual Consumer Version, n.d.). However, a conservative alternative involves the use of PRP, which contains a combination of growth factors and chemokines that stimulate the migration of white blood cells (Pavlovic et al., 2016). When PRP is paired with prolotherapy, the injection of an irritant such as dextrose solution to encourage localized inflammation triggers the body’s natural healing processes (Ryu et al., 2018). Dextrose is seen by the body as a threat or injury, hence causing the body to trigger immune and healing responses (Cleveland Clinic, n.d.). There are many advantages to choosing a non-surgical route such as PRP as to choosing surgery (Dr. Swagatesh Bastia, 2023).
- Low effect on lifestyle : With all non-surgical routes, there are less impacts on life such as risk of complications or less recovery time versus surgery.
- Natural Regeneration: This treatment focuses on stimulating the body’s own healing mechanisms, promoting tissue repair and regeneration.
- Reduced Pain : The majority of the time, patients experience less pain and discomfort compared to surgical options.
- Improved Recovery : Recovery time is typically decreased, and patients can return to activity sooner
- Lower Cost : PRP and Prolotherapy is a non-surgical option, making it cheaper than actual surgery
- Long-Term Benefits : PRP with Prolotherapy not only addresses the ACL injury but also helps with degenerative changes in the knee. It promotes overall knee health and reduces the risk of future injuries such as arthritis.
- The Manufacturing of PRP
In the medical world, it is standard that centrifugation is used to isolate different cell components from their medium (Mohammad Sharifian Gh and Fatemeh Norouzi, 2023). Essentially without delving into the calculations and factors such as temperature, viscosity and more, an initial centrifugation is performed to separate the red blood cells from the white blood cells followed by a second centrifugation with the goal of concentrating the platelets (Dhurat and Sukesh, 2014).
The first spin is performed at constant acceleration to separate the red blood cells from the rest of the blood (Dhurat and Sukesh, 2014). After the initial spin, the blood separates into three parts. An upper layer containing mostly white blood cells and platelets, a middle layer known as the buffy coat consisting of mostly white blood cells and a bottom layer consisting mainly of red blood cells. There are many variations of PRP such as P-PRP or leukocyte poor (little white blood cells) and L-PRP (leukocyte rich, many white blood cells) and L-PRP is known to cause inflammation but not limited to that, it can also cause catabolism which can break down molecules such as collagen, which is why P-PRP is viewed as a more effective method for healing as inflammation can be induced from prolotherapy, meaning an alternative route can be taken to avoid the negative perks of L-PRP (Wang et al., 2018)(Lana et al., 2019).
The second spin is harder and faster with the goal of concentrating the platelets (Dhurat and Sukesh, 2014). Once finished, there are two layers created. The bottom 1/3 is PRP and the upper 2/3rds is PPP (platelet-poor-plasma). The PPP is then removed and the platelets are suspended into a minimum quantity (2-4ml) of plasma and shaken, creating PRP. (Refer to Fig. 1)
Figure 1: The process of PRP with pictures. (Dhurat and Sukesh, 2014)
- The Effect of PRP and How it Induces Recovery
Once injected into the target site, the growth factors and other biological materials such as chemokines help to heal the tendon (Everts et al., 2020). Whilst poor in leukocytes, there are still leukocytes such as neutrophils and monocytes. These leukocytes increase the amount of collagen protein production through increases in procollagen expression (Yuan, Zhang and Wang, 2013). There are many different growth factors including PDGF, TGF-β, VEGF, IGF, HGF, EGF, and bFGF which all contribute to recovery in different ways. For example, TGF-β which exists in platelets helps with tendon healing, collagen production and the reduction of scar tissue. Each of these growth factors have a different respective impact, but they each all contribute to the healing. One of the best parts is that these growth factors come from different parts of the blood, meaning there is no chance of the body rejecting these because they are made from each different patient.
- Conclusion
All types of PRP have the potential to help many people who suffer from tendon damage or conditions such as tendinitis, arthritis and wear and tears (Wang, 2014). With the help of growth factors and chemokines which call more white blood cells to the site of injury, the body is able to non-surgically fix tears without scar tissue (Yuan, Zhang and Wang, 2013). PRP comes with many other benefits such as the relative safety of the injection and low pain compared to surgery (Dr. Swagatesh Bastia, 2023). The best part, however, is how fast and easy it is to make PRP and how powerful it is even though it can be made in half an hour (Dhurat and Sukesh, 2014). When combined with other techniques that speed up healing such as prolotherapy, healing times can be reduced and pain can be decreased (Dr. Swagatesh Bastia, 2023).
Citations
American Red Cross (2022). What Are Platelets In Blood. [online] www.redcrossblood.org. Available at: https://www.redcrossblood.org/donate-blood/dlp/platelet-information.html#:~:text=Platelets%2C%20or%20thrombocytes%2C%20are%20small.
Cleveland Clinic. (n.d.). Platelet-Rich Plasma (PRP): Uses & Procedure Details. [online] Available at: https://my.clevelandclinic.org/health/treatments/21102-platelet-rich-plasma.
Cleveland Clinic. (n.d.). Prolotherapy: What It Is, Uses & Side Effects. [online] Available at: https://my.clevelandclinic.org/health/treatments/22426-prolotherapy.
Dhurat, R. and Sukesh, M. (2014). Principles and methods of preparation of platelet-rich plasma: A review and author′s perspective. Journal of Cutaneous and Aesthetic Surgery, [online] 7(4), p.189. doi:https://doi.org/10.4103/0974-2077.150734.
Dohan Ehrenfest, D.M., Andia, I., Zumstein, M.A., Zhang, C.-Q., Pinto, N.R. and Bielecki, T. (2014). Classification of platelet concentrates (Platelet-Rich Plasma-PRP, Platelet-Rich Fibrin-PRF) for topical and infiltrative use in orthopedic and sports medicine: current consensus, clinical implications and perspectives. Muscles, Ligaments and Tendons Journal, [online] 4(1), pp.3–9. Available at: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4049647/.
Dr. Swagatesh Bastia (2023). ACL tear treatment without surgery | PRP with Prolotherapy. [online] Alleviate pain clinic. Available at: https://www.alleviatepainclinic.com/blog/treating-partial-aclanterior-cruciate-ligament-tears-without-surgery-the-power-of-prp-with-prolotherapy/#:~:text=PRP%20is%20a%20concentrated%20solution [Accessed 16 Aug. 2024].
Everts, P., Onishi, K., Jayaram, P., Lana, J.F. and Mautner, K. (2020). Platelet-Rich Plasma: New Performance Understandings and Therapeutic Considerations in 2020. International Journal of Molecular Sciences, 21(20), p.7794. doi:https://doi.org/10.3390/ijms21207794.
Hopkinsmedicine.org. (2023). Platelet-Rich Plasma (PRP) Injections. [online] Available at: https://www.hopkinsmedicine.org/health/treatment-tests-and-therapies/plateletrich-plasma-prp-treatment#:~:text=To%20create%20platelet-rich%20plasma [Accessed 16 Aug. 2024].
Hughes, C.E. and Nibbs, R.J.B. (2018). A guide to chemokines and their receptors. The Febs Journal, [online] 285(16), pp.2944–2971. doi:https://doi.org/10.1111/febs.14466.
Joshuaharrismd.com. (2024). PRP Therapy for Tendon Injuries: Joshua D. Harris, MD: Orthopaedic Surgery. [online] Available at: https://www.joshuaharrismd.com/blog/prp-therapy-for-tendon-injuries#:~:text=PRP%20and%20tendon%20injuries [Accessed 16 Aug. 2024].
Lana, J.F., Huber, S.C., Purita, J., Tambeli, C.H., Santos, G.S., Paulus, C. and Annichino-Bizzacchi, J.M. (2019). Leukocyte-rich PRP versus leukocyte-poor PRP – The role of monocyte/macrophage function in the healing cascade. Journal of Clinical Orthopaedics and Trauma, 10, pp.S7–S12. doi:https://doi.org/10.1016/j.jcot.2019.05.008.
Matthewpifermd.com. (2024). How PRP Can Treat Your Arthritis: Dr. Matthew Pifer: Orthopedic Shoulder Surgeon. [online] Available at: https://www.matthewpifermd.com/blog/how-prp-can-treat-your-arthritis#:~:text=PRP%20not%20only%20relieves%20pain [Accessed 16 Aug. 2024].
Mohammad Sharifian Gh and Fatemeh Norouzi (2023). Guidelines for an optimized differential centrifugation of cells. Biochemistry and Biophysics Reports, 36, pp.101585–101585. doi:https://doi.org/10.1016/j.bbrep.2023.101585.
MSD Manual Consumer Version. (n.d.). Overview of Sprains and Other Soft-Tissue Injuries – Injuries and Poisoning. [online] Available at: https://www.msdmanuals.com/home/injuries-and-poisoning/sprains-and-other-soft-tissue-injuries/overview-of-sprains-and-other-soft-tissue-injuries.
Pavlovic, V., Ciric, M., Jovanovic, V. and Stojanovic, P. (2016). Platelet Rich Plasma: a short overview of certain bioactive components. Open Medicine, 11(1). doi:https://doi.org/10.1515/med-2016-0048.
Platelet-Rich Plasma (PRP) Injection: How It Works | HSS (2015). Platelet-rich Plasma Treatments for injuries. [online] Hospital for Special Surgery. Available at: https://www.hss.edu/condition-list_prp-injections.asp.
Ryu, K., Ko, D., Lim, G., Kim, E. and Lee, S.H. (2018). Ultrasound-Guided Prolotherapy with Polydeoxyribonucleotide for Painful Rotator Cuff Tendinopathy. Pain Research and Management, 2018, pp.1–5. doi:https://doi.org/10.1155/2018/8286190.
Serkan Akpancar and Deniz Gül (2019). Comparison of Platelet Rich Plasma and Prolotherapy in the Management of Osteochondral Lesions of the Talus: A Retrospective Cohort Study. Medical Science Monitor, 25, pp.5640–5647. doi:https://doi.org/10.12659/msm.914111.
Stanford Children’s Health (2019). What is Plasma? [online] Stanfordchildrens.org. Available at: https://www.stanfordchildrens.org/en/topic/default?id=what-is-plasma-160-37.
University of Rochester Medical Center (2019). What Are Platelets? – Health Encyclopedia – University of Rochester Medical Center. [online] Rochester.edu. Available at: https://www.urmc.rochester.edu/encyclopedia/content.aspx?ContentTypeID=160&ContentID=36.
Wang, J.H-C. (2014). Can PRP effectively treat injured tendons? Muscles, Ligaments and Tendons Journal, [online] 4(1), pp.35–37. Available at: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4049648/.
Wang, S., Fan, W., Jia, J., Ma, L., Yu, J. and Wang, C. (2018). Is exclusion of leukocytes from platelet-rich plasma (PRP) a better choice for early intervertebral disc regeneration? Stem Cell Research & Therapy, 9(1). doi:https://doi.org/10.1186/s13287-018-0937-7.
Welcomebackclinic.com. (2024). Prolotherapy with Platelet Rich Plasma – Welcome Back Clinic – MRI and Pain Management Centre. [online] Available at: https://www.welcomebackclinic.com/services/treatment/prolotherapy-platelet-rich-plasma.htm#:~:text=Prolotherapy%20is%20a%20treatment%20that [Accessed 16 Aug. 2024].
Won, S.J., Kim, D. and Kim, J.M. (2022). Effect of platelet-rich plasma injections for chronic nonspecific low back pain. Medicine, [online] 101(8), p.e28935. doi:https://doi.org/10.1097/md.0000000000028935.
Yale Medicine. (n.d.). Platelet-Rich Plasma (PRP) Injections in Sports. [online] Available at: https://www.yalemedicine.org/conditions/platelet-rich-plasma-injections#:~:text=PRP%20is%20a%20therapy%20produced.
Yuan, T., Zhang, C.-Q. and Wang, J.H-C. (2013). Augmenting tendon and ligament repair with platelet-rich plasma (PRP). Muscles, Ligaments and Tendons Journal, [online] 3(3), pp.139–149. Available at: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3838322/.